A treatise on the frequently asked question of the extent to which food supports the health of the process in mental disorders.

The relationship between nutrition and mental disorders has attracted considerable research interest, with studies of various dietary supplements and nutrition to examine interventions. The current evidence shows that certain dietary approaches have moderate benefits, in particular Omega-3 fatty acids and Multi-micronutrient formulations, however, replace these interventions is not a conventional treatments, but can be used in specific cases as useful additions. Major medical organizations take conservative positions and recommend nutritional interventions, mainly in the case of documented defects, or as a complementary approaches under medical supervision. The field requires more rigorous long-term studies, in particular for the identification of individuals who could benefit most from personalized nutrition strategies.
Dietary supplements: an evidence by category
Omega-3 fatty acids lead to the dietary Supplement research with moderate advantages
Mineral Supplement shows potential in the case of deficiency
The research on the mineral Supplement shows different degrees of Evidence with different minerals. Iron supplementation demonstrated the strongest evidence and , in particular, for children with Ferritin-Mirrors below 30 ng/mL. Meta-analyses show consistently that 84% of ADHD children have low iron levels, compared with 18% of the control groups. Zinc Supplement shows mixed results on a global level, but demonstrated efficacy in populations with documented defects, in which therapeutic doses of 30-40mg daily, the necessary stimulants-drugs doses of 20-40% can reduce. The magnesium research remains on Level IV evidence is limited, although children with ADHD show consistently lower Serum magnesium levels.
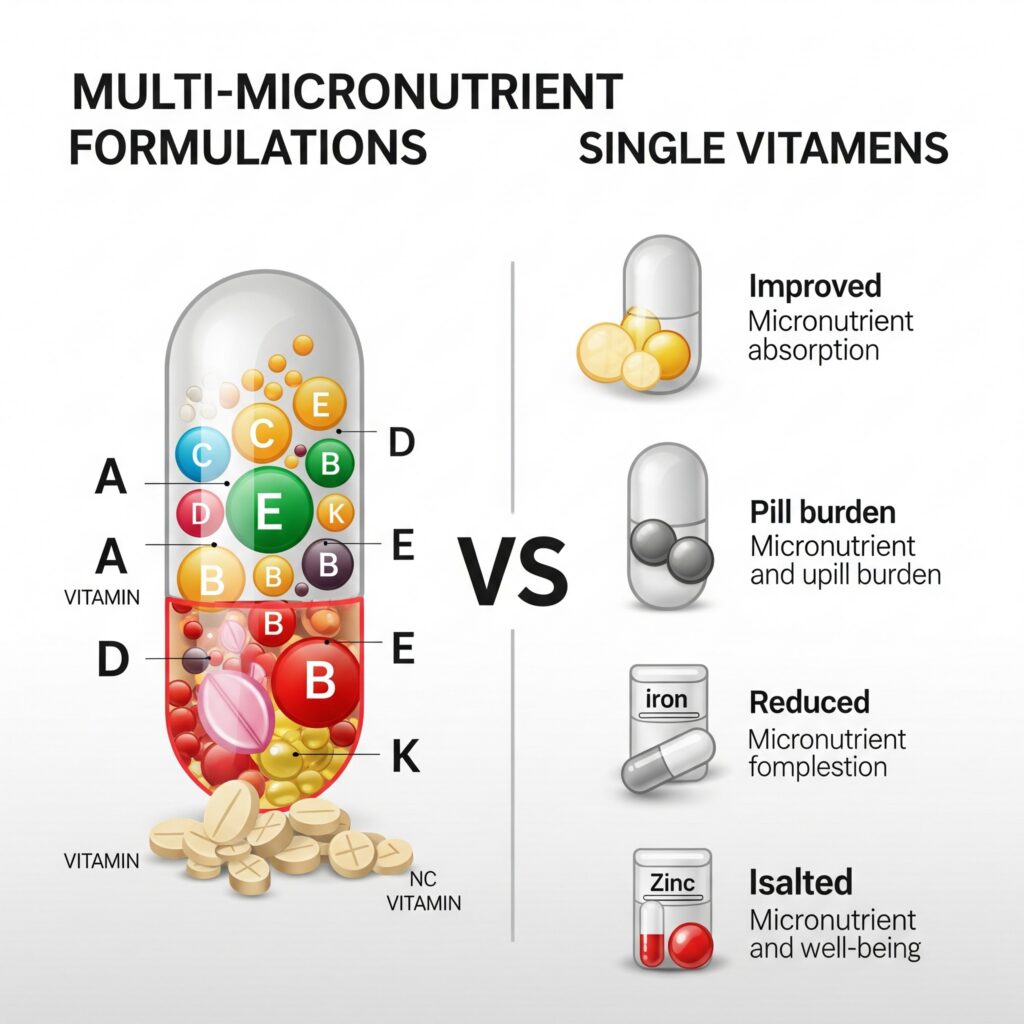
Vitamin Supplement shows limited individual evidence
Individual vitamin supplementation in ADHD shows limited evidence, with most of the positive results of Multi-micronutrient formulations rather than individual vitamins come from. A Landmark study by 2022 demonstrated that broad-spectrum formulations with 36 ingredients, produced a 54%reduction in treatment response rate, compared with 18% for Placebo, with a moderate effect strengths (Cohens d = 0.49 in) for global Work. Vitamin D Supplement shows only in case of documented deficiency, although Meta-analyses show that 84% of children with ADHD, Vitamin D deficiency, compared with 18% of the control groups.
Dietary interventions: Of Elimination to promote
Little-food diets show the greatest effects of the dietary interventions
The oligo antigens or a Little-foods diet (FFD) provides the nutrition intervention with the strongest scientific support and effect, and strengths of 0.51-0.80 Meta-analyses. This highly restrictive approach involves the elimination of most of the food with the exception of rice, meat, vegetables, pears, and water for 4 weeks, followed by a systematic re-introduction. About 60% of the children show significant improvement, with over 40% symptom reduction. The implementation challenges are considerable and require defects intensive family Engagement and professional Monitoring for the prevention of Nutrient.

Artificial additive-Elimination shows small but consistent effects
The Feingold diet, and similar approaches to the elimination of artificial coloring, flavoring and preservatives demonstrate small to moderate benefits with Effect sizes from 0.08 to 0.44 for. Parents reviews show consistently larger effects than teacher ratings, with hyperactivity and impulsivity appeal better than inattention symptoms. Meta-analyses estimate that 10-30% of the children could show measurable improvements, although the clinical significance remains controversial.
General dietary patterns offer protective effects
Mediterranean and DASH eating pattern to show a consistent protective associations with ADHD in observational studies. Children with low Mediterranean diet adherence have 7,07-fold higher chance of an ADHD diagnosis, while high adherence with 51% lower odds is associated. This wholefoods approaches, the fruits, vegetables, whole grains and fish stress and at the same time, processed foods, limit, provide nutritional completeness without the risks of more restrictive diets.
Clinical efficacy after symptom domains
Hyperactivity and impulsivity respond best to dietary interventions
Several dietary supplements and dietary studies across the show hyperactivity and impulsivity symptoms, the most consistent improvements. Omega-3 Supplement is especially targeted to these domains, if EPA exceed doses of 500mg daily. Zinc supplementation demonstrates the primary advantages for hyperactive behaviors, while Little-to produce food diets comprehensive improvements across all symptom domains.
Inattention symptoms require targeted approaches
Inattention symptoms show variable responses to dietary interventions. Iron supplementation produced the strongest effects on attention, especially for children with documented deficiency. Omega-3 fatty acids show mixed results for parent-reported inattention, demonstrate to large Effect sizes for cognitive attention to measurements.
Implementation guidelines, and dosage recommendations
Evidence-based dosing requires individualization
Effective Supplement requires specific dosing strategies based on current evidence. For Omega-3 fatty acids begin to minimal effective doses in 500mg of EPA daily, with optimal results at 1,000-2,000 mg total Omega-3s for a minimum of 12-16 weeks. Multi-micronutrient formulations require 9-12 capsules daily to achieve therapeutic effects. Mineral supplements following weight-based dosages: iron with 3-6mg/kg/day, zinc 15-30mg elemental twice a day.
Biomarker Monitoring improves treatment precision
Laboratory monitoring improves treatment results and safety. Essential reviews include Ferritin level for iron status (the target of >30 ng/mL), 25-Hydroxyvitamin D (>30 ng/mL maintained), erythrocyte Magnesium and Plasma zinc with copper conditions. Baseline Omega-3 Index test can tell the treatment of speech before.
Current medical consensus and guidelines
Large organizations are taking conservative positions
The American Academy of Pediatrics, NICE guidelines and the World Federation of ADHD stress is consistent that dietary interventions insufficient evidence as a primary ADHD treatments have. These organizations recommend focusing on evidence-based pharmacological and behavioral interventions, while dietary approaches to be considered in the case of documented defects or carefully monitored adjuvant treatments can be considered.
Integration with conventional treatment shows potential
Clinical guidelines support nutrition interventions primarily as a complementary approaches rather than as a replacement for the standard treatment. For adjuvant use, some families report on the ability to reduce medication doses, while the symptom control in an upright position.

Safety profiles and clinical Considerations
Most of the supplements to demonstrate a good safety profile
Supplements for ADHD generally show excellent compatibility in comparison to pharmaceutical options. Omega-3 fatty acids mainly produce mild gastrointestinal effects, while right cause under-dosed minerals rare but significant side effects. Iron supplementation, however, requires careful Monitoring because of the risk of poisoning.
Elimination diets mountains nutrition risks
Restrictive dietary interventions mountains considerable risks of nutrient deficiencies, especially for growing children. Little-food diets of the main food groups are eliminated and can affect growth, bone health and cognitive development without proper supplementation.
Conclusion
The scientific evidence for nutritional supplements and dietary interventions in ADHD shows a complex landscape of moderate benefits, implementation challenges, and significant gaps in the Research. While Omega-3 fatty acids and Multi-micronutrient-point formulations with the most potential to not be able to replace these interventions evidence-based conventional treatments. The current medical consensus emphasizes appropriate nutrition approaches as adjuvant strategies, in particular for persons with documented defects or complementary options under the professional supervision are looking for.